What does Biotin do to our metabolic activities?
Biotin is a water-soluble B vitamin, also known as Vitamin B7 or Vitamin H. Biotin is an essential micronutrient for mammals that plays a key role in metabolism of fats, carbohydrates and proteins in our body.
How biotin plays its role?
Biotin acts as a covalently bound coenzyme for five carboxylases, those are acetyl-CoA carboxylases 1 and 2, propionyl –CoA carboxylase (PCC), 3-methylcrotonyl-CoA carboxylase (MCC) and pyruvate carboxylase. These are key enzymes in metabolism of fatty acids, amino acids and gluconeogenesis, a metabolic pathway that generates glucose from non-carbohydrate carbon substrates [1, 4,5].
DNA studies and gene expression studies suggested that numerous genes are regulated by biotin at the transcriptional and post-transcriptional level. Biotinylation and biotin deficiencies have an impact on turning on or off genes, replication and repair of DNA and response to cell stress.
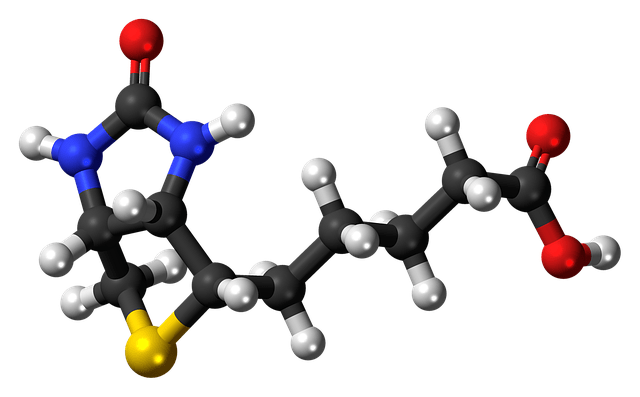
Biotin structure
Source of Biotin: Food
Human body cannot synthesize Biotin. Most healthy individual get the required biotin from Well-balanced diet. Food rich in Biotin are egg, meat, poultry, Fish, cereals, seeds, Nuts and vegetables. Foods that are super rich in Biotin are
- egg yolk
- beef liver
- salmon fish
- pork
- sunflower seeds
- sweet potato
- Almonds
- Spinach
- Broccoli
Raw egg white contain Biotin binding protein called avidin, which decreases the bioavailability of Biotin. Cooking the egg prevent this Biotin loss [2,4]. It is also found that gut microbes also capable of synthesizing biotin but its contribution to the body is not well known [10].
Recommended intake:
It is evident that dietary biotin is 100% bioavailable.
Recommended dietary allowance (RDA) of Biotin is not established yet, due to the insufficient evidence. Recommendation for adequate intake (AI) are based on the average intake of biotin in an apparently healthy population. The AI for biotin is 30 mcg in men, women, and pregnant women who are 19 yrs and older and increases to 35 mcg for lactating women[2,4].
Biotin Deficiency:
Biotin deficiencies are generally very rare to occur. Congenital or genetic biotin deficiency is due to autosomal recessive disorder, which leads to the dysfunction of either holocarboxylase synthase (HLCS) or biotinidase. Holocarboxylase synthetase (HLCS) is a key enzyme that play a pivotal role in biotin-dependent metabolic pathways. It is found to catalyses the binding of biotin to all 5 carboxylases. HLCS is also to found to participate in gene regulation at the chromatin level. Biotinidase is an enzyme that catalyse the release of biotin from break-down products of carboxylases and hence its important in biotin recycling [1,4,5]. When it occurs within the first 6 weeks of life, it is known as neonatal type and in this deficiency the enzyme holocarboxylase synthetase is absent and patients typically have severe, life threatening conditions. Past 3 months of life, the infantile form predominates and is defined by a biotinidase deficiency.
Acquired biotin deficiency commonly caused by the raw egg consumption. The protein Avidin in raw egg whites bind to biotin tightly thus preventing it from being used by the body. Other reasons for deficiency may be due to taking anticonvulsant medications, such as valproic acid. Alcoholism, pregnancy, prolonged use of antibiotics which affects normal gut flora can also be the causes for acquired biotin deficiency [3].
Symptoms of biotin deficiency [3]:
Either acquired or congenital, symptoms for Biotin deficiency includes:
- Alopecia
- Eczematous skin rashes
- Seborrheic dermatitis
- Conjunctivitis
- Neurological symptoms occurs at more severe levels, which includes depression, lethargy, hypotonia and seizures. Generally, dermatological manifestation appears first in biotin deficiency and thus it is an important indicator.
Biotin supplementation:
There are no established studies that the healthy human with balanced diet are deficient for biotin. Typical dietary intake of biotin in western population is estimated to be between 35 and 70 mcg/day.
Pharmacological doses of biotin supplementation is being recommended for frank biotin deficiency. It is observe in individuals who have mutation in HLCS, biotinidase and in people who consumes large amount of raw egg whites [3,5].
Biotin Supplementation for hair and nail growth:
Since Biotin is necessary for keratin production, it is considered important in promoting the Hair and nail growth. Till date there are no clinical trials supporting that biotin supplementation helps in improving the quality of hair and nail growth, but there is a study which showed 18 reported cases of biotin use for hair and nail growth changes the quality. In all cases, patients receiving biotin supplementation had an underlying pathology for poor hair or nail growth. All cases showed evidence of clinical improvement after receiving biotin[3,6].

As said earlier for acquired and inherited causes of biotin deficiency and for some conditions, such as brittle nail syndrome or uncombable hair syndrome which is characterised by dry, frizzy, straw-coloured or silvery-blond hair, biotin supplementation may help and benefit [11,3,6]. However, healthy people need to take doctor advice before taking Biotin supplementation since no trials proves biotin efficacy in healthy individuals.
Toxicity:
As far as reported, there are no toxicities associated with excess biotin intake. Food and Drug Administration (FDA) warning stated that biotin might interfere with laboratory tests leading to incorrect diagnoses. According to the case studies and in vivo studies shows that ingestion of biotin supplement interfere with the results of biotinylated immunoasssays. Thyroid test, endocrine test are some of the test that might be interfered by biotin supplements [12,6,3].
Pregnancy and Biotin deficiency:
Pregnancy and lactation increases the demand for the biotin. Studies found that despite of dietary intake, there is a marginal biotin deficiency found in pregnant women. Studies suggest that increase in the biotin intake during pregnancy is likely needed, when there is a marginal biotin deficiency [5].
Diabetes and Biotin:
Animal studies suggest that high dose of biotin helps in controlling the diabetes and certain diabetic complications. Further studies are warranted to this association of Diabetes to Biotin.
Take away points:
- Biotin is a water-soluble vitamin, which is essential for metabolism of fats, proteins and carbohydrates.
- Biotin deficiency is very rare, If biotin deficiency occurs, biotin rich foods helps and biotin supplements has to be taken based on doctor’s advice.
Reference:
- Teo Soleymani MD, et al. The Infatuation With Biotin Supplementation: Is There Truth Behind Its Rising Popularity? A Comparative Analysis Of Clinical Efficacy Versus Social Popularity. J Drugs Dermatol. 2017;16(5):496-500.
- https://ods.od.nih.gov/factsheets/Biotin-HealthProfessional/
- Deepa P. Patel, Shane M. Swink, Leslie Castelo-Soccio, A Review of the Use of Biotin for Hair Loss. Skin Appendage Disord 2017; 3:166–169. DOI: 10.1159/000462981.
- Zempleni J, Kuroishi T. Biotin. Adv Nutr. 2012;3(2):213-214. Published 2012 Mar 1. doi:10.3945/an.111.001305.
- Donald M Mock, Biotin: From Nutrition to Therapeutics. J Nutr 2017; 147:1487–92.
- Jason J. John and Shari R. Lipner, Consumer Perception of Biotin Supplementation. Journal of Cutaneous Medicine and Surgery 2019, Vol. 23(6) 613–616. DOI: 10.1177/1203475419871046.
- Shari R. Lipner & Richard K. Scher (2018) Biotin for the treatment of nail disease: what is the evidence?, Journal of Dermatological Treatment, 29:4, 411-414, DOI: 10.1080/09546634.2017.1395799 [Pubmed abstract].
- Jason J John , Victoria Cooley , Shari R Lipner, Assessment of biotin supplementation among patients in an outpatient dermatology clinic. J Am Acad Dermatol 2019 Aug; 81(2):620-621. doi: 0.1016/j.jaad.2018.12.045. Epub 2019 Jan 8.
- Rocio Rodriguez-Melendeza, Janos Zemplenia, Regulation of gene expression by biotin_ (Review). Journal of Nutritional Biochemistry 14 (2003) 680–690.
- Ian Rowland · Glenn Gibson, et al. Gut microbiota functions: metabolism of nutrients and other food components. Eur J Nutr (2018) 57:1–24 DOI 10.1007/s00394-017-1445-8.
- Pamela Calderon , Nina Otberg, Jerry Shapiro, Uncombable hair syndrome. J Am Acad Dermatol . 2009 Sep;61(3):512-5. doi: 10.1016/j.jaad.2009.01.006.
- Mark F. McCarty B.A. In type 1 diabetics, high-dose biotin may compensate for low hepatic insulin exposure, promoting a more normal expression of glycolytic and gluconeogenic enyzymes and thereby aiding glycemic control. Medical Hypotheses 95 (2016) 45–48.
- US Food and Drug Administration. The FDA warns that biotin may interfere with lab tests: FDA safety communication. https://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm586505.htm. Accessed September 3, 2018.